Dr. Friedman's Office: (210) 880-3000
Diabetic Retinopathy
Diabetes is a disease that is growing in prevalence year by year. I would bet that many people reading this article would know someone that is a diabetic or at least a “pre-diabetic”. Whether it is due to poor diet and lifestyle or just because they stopped producing enough insulin to keep their blood sugar under control, people with diabetes have a systemic disease that affects all parts of the body.
The eyes are no exception to this rule. Although diabetes does affect larger organs - the leading causes of death in people with diabetes are heart attack and stroke – diabetes has an especially negative effect on parts of the body with small blood vessels including the kidneys, peripheral nerves, and the eyes. People with diabetes can have profound vision loss due to the effects of the disease. This is called diabetic retinopathy.
HOW DIABETES AFFECTS YOUR EYES
There are 3 main ways that diabetes can show up in the eye and affect the vision: proliferative diabetic retinopathy, macular edema, and retinal ischemia.
As I like to tell my patients, the trouble with diabetic eyes is that they are not getting enough oxygen and nutrition due to poor blood flow. Naturally, the eye responds by building new pathways for blood to get to the retina. It builds miniature blood vessels that get the job done quickly. Unfortunately, this is like hiring a shoddy construction company. They get the job done, but soon after, these blood vessels break down, bleed, and can form scar tissue. (See Figure) This becomes problematic as the blood can block vision and the scar tissue can cause retinal detachments. Both of these problems make it extremely hard to see.
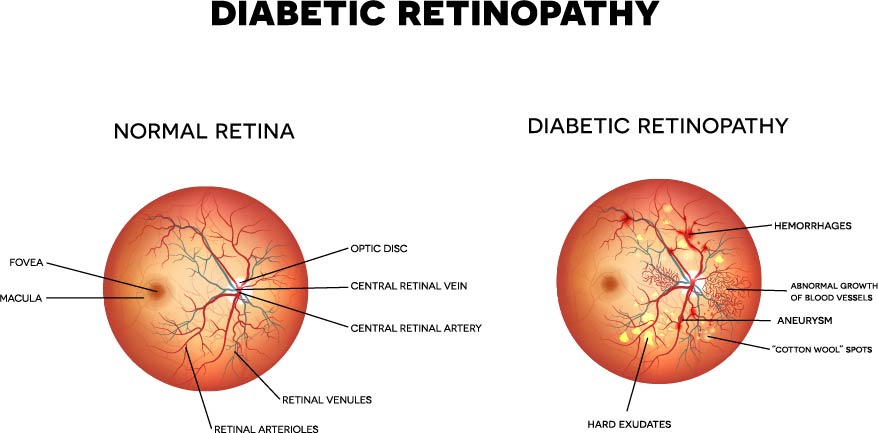
Another way that diabetes can affect the eyes is by making the area around the center of vision (the fovea) fill up with fluid. The blood vessels around this area become extremely leaky and can cause splitting of the retinal layers such that they do not communicate well. This problem is known as diabetic macular edema and can also have a profound effect on vision.
Finally, even if there is no blood or fluid causing problems with the retina and vision, the lack of good blood flow can cause the retina to die (known as retinal ischemia). Unfortunately, when the retina has poor blood flow for a prolonged period of time, it is hard to get it to function again, no matter what we do.
SCREENING IS THE BEST TOOL
So what should you do about your eyes if you have diabetes? The first thing I emphasize is that diabetes is a SYSTEMIC disease. That means, the best means of controlling diabetic retinopathy is to control the underlying diabetes. That means having serious, and possibly frequent, talks with your primary care physician to get your blood sugar levels under control. That also means being aware of your diabetes and checking your blood sugars yourself. I would also recommend you try and learn what your most recent hemoglobin A1c level (this is an average for your blood sugars over the past 3 months). This helps your primary care doctor as well as your ophthalmologist know how well controlled your diabetes is. As for treating the underlying diabetes, some diabetics can control their sugar levels with simple diet and exercise. Some require medications by mouth, and others require supplemental insulin.
With regard to diabetic eye care, you should have a dilated eye exam at least once a year to determine if diabetes is affecting your eyes. You might not know that you have diabetic retinopathy, but your eye care provider can look and tell you if there are any early signs of change. Sometimes, people with diabetic retinopathy require more than one exam per year in order to ensure that the disease is not progressing rapidly to a point where it cannot be treated. Your doctor will need to do a dilated eye exam to see all aspects of the retina. During your eye exam, you will also likely be tested with a machine called an OCT (which stands for optical coherence tomography). This helps determine if there is fluid near the center of vision causing macular edema. Further, you might also receive a test called fluorescein angiography. This shows leaking blood vessels in the retina which could cause potential problems. Both of these tests are very helpful in determining the extent of diabetic eye disease.
Many people with diabetes simply have background diabetic retinopathy. Although there have been changes to the blood vessels, scar tissue and new blood vessels have not started to form. If this is the case, then simply keeping a close watch on the retinas is all that is needed. Depending on how severe the “background” disease is, your eye care provider will tell you how often you have to be examined. Sometimes this is every three months, and sometimes it is once a year.
THE GOOD NEWS IS THAT THERE ARE TREATMENTS
For diabetics with macular edema that has started to affect or threatens the center of vision, there are methods to control the leaky blood vessels. One of the main problems causing the blood vessels to leak is a chemical messenger in the eye called vascular endothelial growth factor (VEGF). Fortunately, there are anti-VEGF medicines that can stop this chemical messenger from reaching its target. These medicines (i.e., Avastin, Eylea, and Lucentis) are all injections that are placed into the back of the eye on a regular basis to close off the leaky vessels. There has also been a recent surge in the use of steroids in and around the eye to fight macular edema. I will be writing more about the benefits and risks of each of these medicines in another article, but for now, know that these medicines require you to have monthly injections as they wear off (much like any other medicine you take).
Another option for diabetic edema is focal laser therapy. In focal laser therapy. This was the tried and true method used until the anti-VEGF medicines were introduced to the market to combat macular edema. Using a low-powered laser, and guided by fluorescein angiography, an ophthalmologist can effectively close off the culprit blood vessels that are leaking and causing the retina to swell. Usually, this laser procedure is very quick and the patients that I have seen very rarely complain about pain. The effects of the laser should be permanent, but they can take 3 or more months to actually start to take effect. A combination of injections and laser is currently the standard of care endorsed by most retina specialists.
Proliferative diabetic retinopathy is an eye disease that causes the formation of new blood vessels in the eye. As I said, these blood vessels are bad news as they can have some severe and lasting effects on vision. The first line of treatment when diabetics show signs of proliferation is to treat with a different variety of laser. A treatment known as pan-retinal photocoagulation (PRP) is used to make the bad blood vessels go away. Essentially, the laser treatment burns the retina that isn’t getting enough oxygen, thereby decreasing the amount of VEGF in the eye. Again, the effects of the laser can take 3 or more months to occur, but as long as no significant scar tissue exists, most diabetics end up doing well. This laser treatment can take a while to complete and might even be done in 2 or more sessions depending on patient comfort.
The treatment is more involved for people with severe diabetes causing bleeding or scar tissue that pulls the retina off the back of the eye (causing a retinal detachment). In these situations, it is usually necessary to perform vitrectomy surgery. A vitrectomy should be done by a retina specialist that is familiar with this type of treatment. During this surgery, the gel (called the vitreous) that fills the eye is removed along with the scar tissue and a saltwater solution is placed in the eye. This effectively gets rid of the scaffold that the scar tissue is growing on and gets rid of any tension that is ripping the fragile blood vessels open. It is also likely during this surgery that you will receive laser PRP and maybe even an anti-VEGF medication.
IN SUMMARY
As you can tell from the flow of this article, getting to the root of the problem ahead of schedule and not letting it get out of hand is the most important thing you can do. The best possible treatment for diabetic retinopathy is to treat the underlying diabetes and keep it under control. This, along with routine screening, will hopefully keep most people from progressing to more severe forms of disease.
I hope this helps in understanding the basics of diabetic eye disease. Again, it is a very involved subject, so please, if you have any more specific questions, please do not hesitate to contact us at sanantonioeyedoctormd@gmail.com.
Duncan Friedman
Retina Specialist
San Antonio, Texas