Dr. Friedman's Office: (210) 880-3000
Glaucoma
Why the heck are eye doctors so insistent that everybody get a dilated eye exam every year? Wouldn’t you notice if you were losing your vision? In my years of dealing with eye disease, I have come to an important conclusion: some eye diseases, such as glaucoma, are sneaky!
I say this because it is an eye disease that hides from many well trained detectives. There are multiple tests and examinations to determine if a patient even has the beginnings of glaucoma. Further, its effects are serious . . . left untreated, glaucoma can cause blind spots and even complete blindness.
The Basics
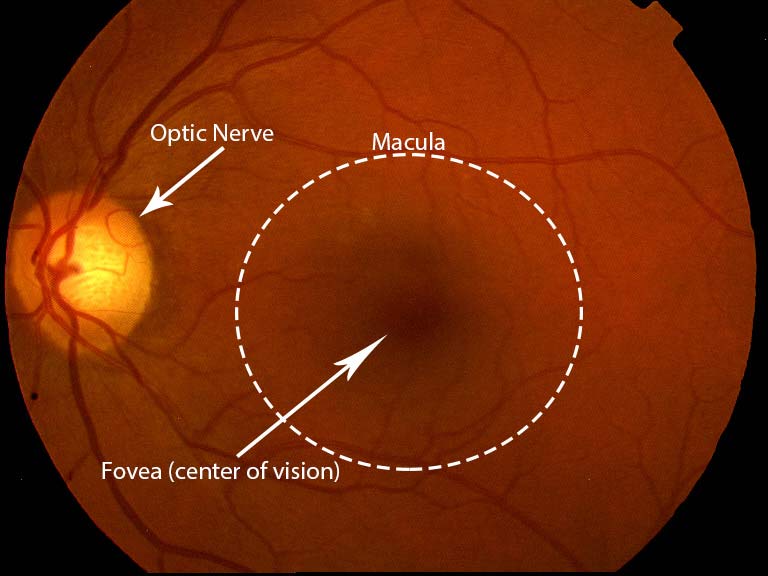
Here is what I can tell you about glaucoma. Glaucoma is a disease affecting the optic nerve in the back of the eye that causes part of the optic nerve to die. It is most often (but not always) caused by high pressure in the eye, and this is why eye care providers are always checking eye pressures. Below is a discussion of the most common type of glaucoma: open angle glaucoma. There are many types of glaucoma, and I will devote other sections of this website to them in the future.
The best way I can relate glaucoma is through two analogies:
First, imagine that you have a bathtub that is constantly filling up with water from the faucet. The bathtub also has a drain that is constantly letting water flow out. If either the faucet is running too fast or the drain gets clogged, the bathtub will fill up and overflow with water. This is a bad thing. Your eye is similar to this bathtub because it is constantly producing fluid (called aqueous humor), and at the same time, it is constantly draining fluid through the part of the eye called “the angle”. If the eye produces too much fluid and the angle cannot drain it out fast enough, the pressure in the eye starts to go up. More on this later . . .
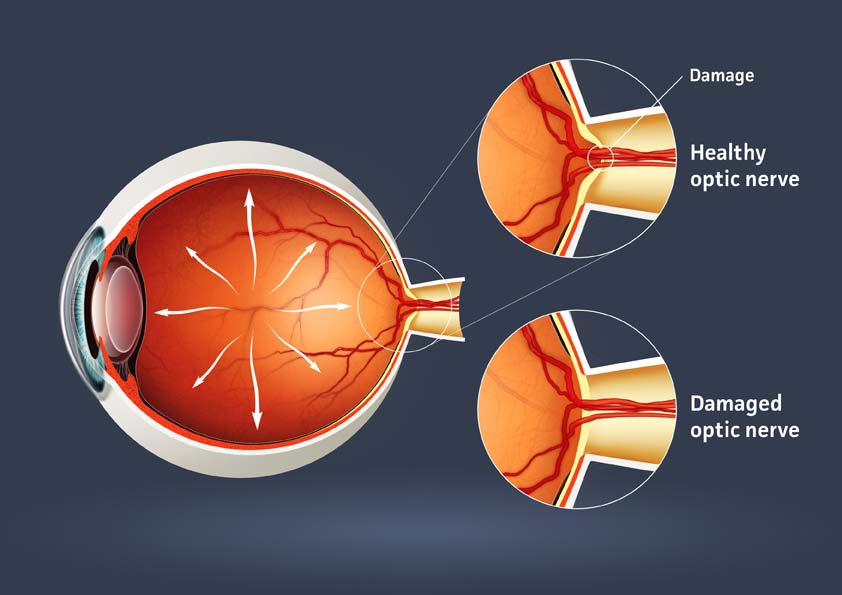
Now, think of all the times that you put too much pressure on a nerve in your body. The most common example is when you get up from sitting too long and you experience “pins and needles” in your leg. This is a result of putting too much pressure on the nerves in your leg. The nerves in your leg recover after a little bit, but you lose feeling for a short amount of time. If you put a lot of pressure on your leg for months and months and months, the nerves would never recover.
Finally, imagine that you are putting pressure on the optic nerve all day long because there is always too much fluid inside the eye. After months and years of pressure, the optic nerve at the back of the eye starts to die. When this happens, you lose vision. These, in a simplified form . . . are the basics of glaucoma.
So how do I know if I have glaucoma?
The fact of the matter is that glaucoma is probably the most mind-boggling and infuriating eye disease (at least to me) because it usually takes multiple visits and many tests to tell whether a person has the early signs of glaucoma. In the realm of eye disease, where most diagnoses are simple, straightforward, and apparent, glaucoma can hide and cause damage without a diagonsis until most of the vision is gone.
That said, your eye care provider will likely need to see you multiple times to determine if your optic nerve has experienced any damage. This can be done by measuring the eye pressure, checking your peripheral vision, looking at the optic nerve with a microscope or pictures, and imaging the optic nerve head using machines that use optical coherence tomography (OCT) scanning. They will also likely need to check the drainage system of the eye using a contact lens to make sure that it is open and not clogged. Again, to arrive at a diagnosis of glaucoma, it might take multiple visits to see if a healthy nerve is experiencing damage over time.
As I hinted at the beginning of this article, some people are more prone to glaucoma than others. Anybody that has a family history of glaucoma is at risk as the majority of common glaucomas have a genetic basis. Further, if you have diabetes, there is an increased risk for glaucoma. Other risk factors that can lead to glaucoma include age (usually people over 65), high eye pressure, African or Hispanic ancestry, farsightedness or nearsightedness, previous eye injury, and systemic health problems such as migraines or poor circulation. If you have any of these in your medical history, you should be examined by an eye doctor that can diagnose and treat glaucoma.
Otherwise, if you are between 20 to 64 years old without any risk factors, your first glaucoma screening can wait until you are 40 years old. If there are no signs at this time, your doctor might only check every couple of years. After 65 (since glaucoma is related to age) it is a good idea to get a yearly screening to make sure that there is no underlying progression that you could be missing . . .
Which brings us to our original point . . .
“Doc, wouldn’t I know if I was losing vision from glaucoma?”
Here is what I don’t like about glaucoma . . . it is sneaky. In ophthalmology, glaucoma is known as “the thief in the night”. It robs you of your vision without you knowing it until it is too late. The parts of the optic nerve that are most damaged early on are your peripheral vision nerve fibers. Since you have two good eyes are that are usually compensating for each other, you wouldn’t necessarily note a blind spot in your peripheral vision.
A glaucoma specialist, friend of mine puts it this way: "I like to think of the eye, optic nerve, and brain as similar to a digital camera system. The eye is the digital camera, the brain is the computer hard drive and the optic nerve is the cord that connects the camera to the hard drive. If the cord is damaged, then the image from the digital camera can’t be uploaded to the hard drive to be seen, even if the camera and hard drive are working well. In glaucoma, as the optic nerve becomes damaged, the images from the eye can’t be uploaded to the brain to be seen. This results in “blind spots” in your vision."
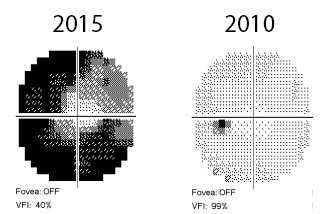
As more and more parts of the optic nerve die, the blind spots get bigger and bigger, but most people do not realize that their vision is disappearing until they have only a little bit of central vision remaining. Further, once the vision is gone, there is no way to rebuild the nerves, so the vision loss is permanent. You can see how serious this disease is. This is why we like to treat glaucoma before it gets too far advanced.
So what can be done about this treacherous disease?
Fortunately, most people that we suspect have glaucoma do not lose a lot of vision because we have means of controlling the pressure in the eye and glaucoma damage progresses very slowly over months and years. As stated earlier, if the eye pressure is constantly high, the optic nerve experiences damage. Although this is not always the hard and fast cure for ALL types of glaucoma, it is a pretty good means to manage the damage from most types of glaucoma. The different ways of treating glaucoma include medications, laser therapy, and surgery.
Most people with open angle glaucoma start out with eye drops to help lower the pressure. There are many different types of drops that work in different ways. Coming back to the bathtub analogy, some drops help by turning the faucet lower causing the eye to fill up slower. Other drops help open up the drainage system, allowing the pressure in the eye to fall. If you are being treated for glaucoma, you might have many different types of drops to use to achieve this goal.
I have to emphasize, as with any medication, if you stop taking it or forget to take a dose, it stops working. Therefore, it is extremely important that you take the medications as instructed. Further, all glaucoma medications have side effects. Certain glaucoma medications can cause eye problems such as burning or itching, redness, dry eyes, change in eye color and eyelash growth. They can also affect the body, causing changes to the heart rate, changes to breathing, dry mouth, and decreased energy. If you experience any of these symptoms, you need to notify your eye doctor so they can modify the medications.
For people that have a lot of eye drops, or if the eye drops are not keeping the pressure low enough, laser therapy is an option. Your ophthalmologist can consider using a specialized laser to help open the drainage system in the eye. Usually, it only takes one or two treatments with this special laser (known as trabeculoplasty) to help lower pressure.
Unfortunately, there are certain people with glaucoma that have high eye pressures despite these initial interventions. In these people, the damage to the optic nerve is likely to progress without surgery. The essence of glaucoma surgery is to build an additional drain to allow the fluid to flow out of the eye since the normal drainage system is no longer working. Sometimes this involves making a “filter” on the eye wall, known as trabeculectomy. Other times, your ophthalmologist will put in a stenting device or tube to help drain the excess fluid known as a shunt procedure. Either way, your ophthalmologist will determine when this type of surgery is necessary. There are glaucoma specialists that undergo an extra year of training in this type of surgery and disease management (although all ophthalmologists have basic training in glaucoma diagnosis and treatment).
In summary
Glaucoma is a very serious eye disease that can cause permanent vision loss if it is not detected early. Still, there are excellent treatments available to help halt the progression of glaucoma. A good dilated eye exam by your eye care provider can help determine whether you are at risk for glaucoma and how often you should be screened at future visits.
Glaucoma is a complex disease with many different forms; this article merely addresses diagnosis and treatment of the most common type of glaucoma. If you want to know more or have any specific questions, please contact us at sanantonioeyedoctormd@gmail.com.
Special thanks to Dr. Lindsay Rhodes (glaucoma specialist, Birmingham, Alabama) for her review of this article and particularly the digital camera analogy.
Duncan Friedman, M.D.
Ophthalmologist
San Antonio, Texas